Setting up Insurance Billing for Group vs Individual
This article provides guidance on configuring settings to ensure the appropriate population of either the group NPI or individual NPI in Box #33a of the CMS-1500 form.
When going through the configuration settings in zHealth, there are two places where billing information must be entered for insurance claims.
This is in the “Facility” settings and “Provider” settings.
 Facility Settings
Facility Settings
 To access the facility settings we will navigate to “Update Info”. To access the facility settings we will navigate to “Update Info”. | |
 This is where we will enter in the Organization (Group) NPI. This NPI number is also known as a “Type 2” NPI |
 Provider Settings
Provider Settings
 To access the provider settings we will navigate to “Update Info”.
To access the provider settings we will navigate to “Update Info”. 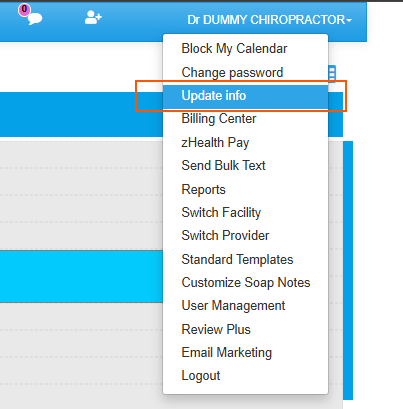
 Once there we will select the “Provider” option and navigate to the “NPI Number” field. This is where the Individual NPI will be entered.
Once there we will select the “Provider” option and navigate to the “NPI Number” field. This is where the Individual NPI will be entered.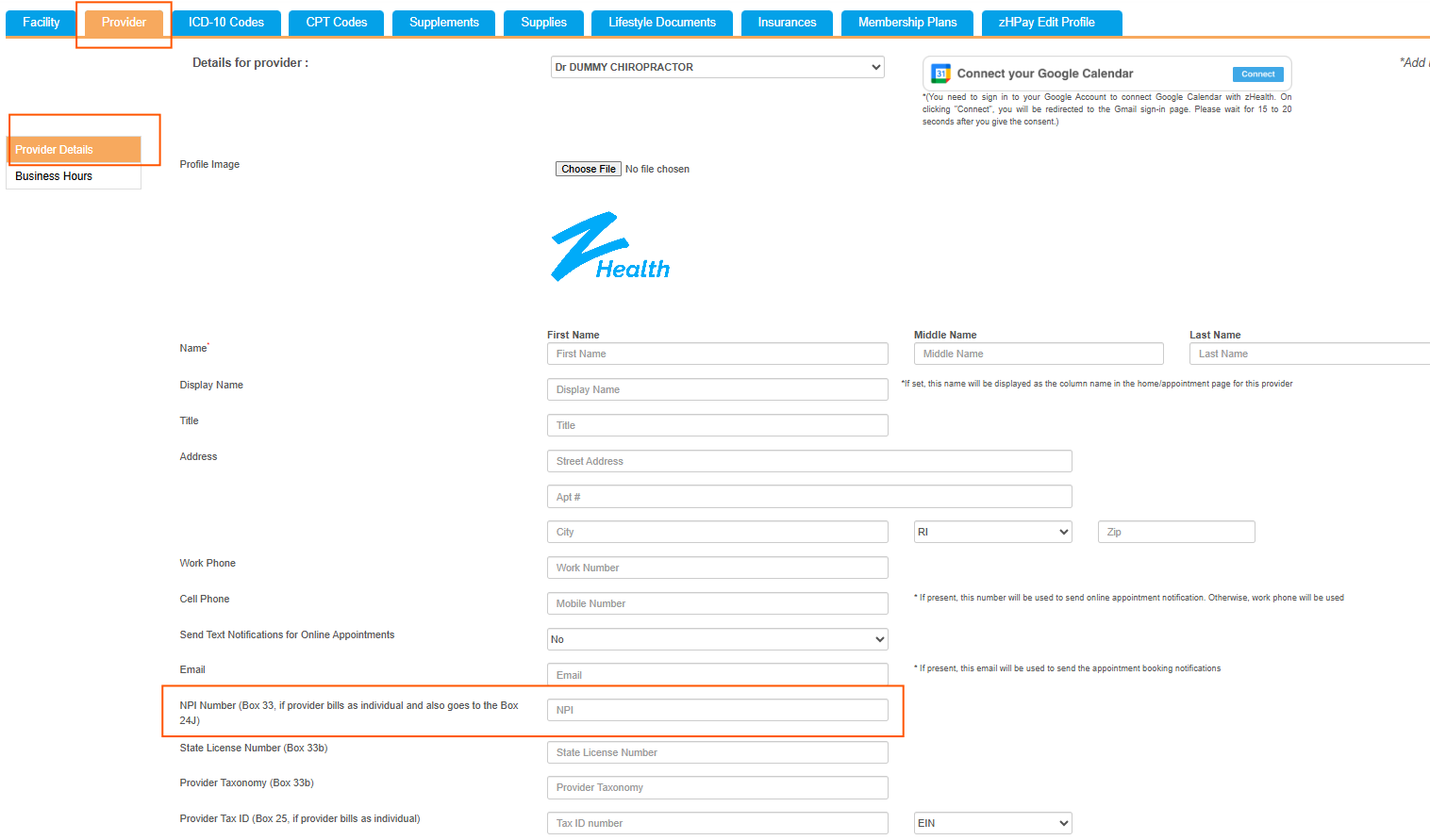

To access the provider settings we will navigate to “Update Info”.

Once there we will select the “Provider” option and navigate to the “NPI Number” field. This is where the Individual NPI will be entered.
 Setting Up Bill by Organization (Group)
Setting Up Bill by Organization (Group)
 Setting Up Bill by Organization (Group)
Setting Up Bill by Organization (Group) In the “Provider” settings, there is a field labeled “Billing Provider Entity Type”. This is how you can set up your zHealth account to bill using the organization’s information, or whether to use the individual provider’s information | |
 By selecting “Individual” you will be using the NPI information given in this “Provider” settings and using that to complete box #33 of the CMS-1500 form. |
 Setting Up Bill by Individual
Setting Up Bill by Individual By selecting “Organization” you will be using the NPI information given in the “Facility Settings” to complete box #33 |
Related Articles
How to Fill the HCFA Claim Form in zHealth
This document only explains what type of information you need to fill in each box in the HCFA (CMS-1500) claim form and where you can add, update, or change corresponding information in your zHealth account to ensure accurate information for claim ...Claim Submission Checklist
The following claim submission checklist will help providers or billers to ensure all necessary (and accurate) information are provided at the time of claim submission. Facility Setup Checklist 1. Verify the following information for each insurance ...Individual Claim Submission in zHealth
Video Demonstrating- How to Submit an Individual Claim In this video, you will learn how you can submit individual claim. <br> A guide providing step-by-step instructions explaining how to submit individual claim The ...Insurance Claim Error Cheat Sheet
In chiropractic billing, claim errors result in either rejections or denials and overcoming these can be challenging. Even small errors like missing or incorrect patient demographic information can lead to claim denials and payment delays. As a ...Tracking Insurance Claim Status
When you submit an electronic claim, the application creates and sends an 837 EDI file to the clearinghouse (Office Ally). After that, you or the system cannot control your claim. Fortunately, the application allows you to track your claim’s status. ...