Using Blue Shield of California’s Claims-Routing Tool
When you send claims, it’s crucial that you understand where the claims should go. It's frustrating for providers when their claims get denied because they selected the incorrect insurance company name when registering a patient or updating their information.
Providers or staff can use Blue Shield of California’s online claims-routing tool to easily determine the correct insurance name, such as Anthem or Blue Cross Cali, and the correct mailing address.
The Claims-Routing Tool is a great tool for verifying if the claim is being routed to the correct claims processing center (whether EDI or paper). Note that this tool is free to use and you don't require to login.
Accessing the Claims-Routing Tool
 1. Go the official website of Blue Shield California. Click the link here to get started. Click the Provider link on the top right corner of the website as shown here. 1. Go the official website of Blue Shield California. Click the link here to get started. Click the Provider link on the top right corner of the website as shown here.
|
|

2. On the Provider page of Blue Shield California, scroll down to the Claims section. Click on the "Claims-Routing Tool" link as shown here.
|
|

3. On the Claims-Routing Tool page, follow the below instructions to get more details about the insurance plan, company name, and address:
a. Enter the three-character alpha prefix* displayed on the Member ID card. b. Enter the date of service (The date can be up to 36 months before and 31 days after the current date).
c. Click the "Search" button.
The result will show where to submit your claim. |
|
*Most Blue Cross and Blue Shield (BCBS) branded ID cards display a three-character alpha prefix in the first three positions of the member’s ID number. The alpha prefix helps you determine insurance eligibility and benefits, and is necessary for proper claim filing.
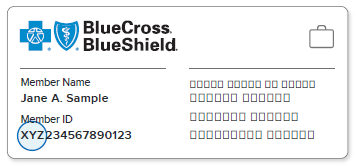
*Federal Employee Program (FEP) members’ ID cards do not have a three-character alpha prefix. Rather, all FEP member identification numbers begin with the letter "R".
Remember: Member ID cards are for identification purposes only; they do not guarantee eligibility or payment of your claim. You should always verify patient eligibility by calling 800-676-BLUE (2583).
Related Article:
Related Articles
Guidelines for Billing BCBS Illinois (HCSC) and Blue Shield of California
According to the Office Ally notification dated 01/13/2025, when submitting claims to the following two payers, the "Service Facility Information" on HCFA/UB claims does not require the Service Facility NPI if it is the same as the Billing Provider ...Batch Generating and Submitting Claims
You can choose to submit all insurance claims at once, allowing you to send claims for multiple patients to their respective insurance providers. This feature in zHealth is a helpful tool that enables you to submit all claims in a single action for ...How to Batch Submit Claims at the Patient Level
You have the option to submit all insurance claims for a given patient at once. This means that you will be sending claims for multiple patient visits to the corresponding insurance providers. This is a useful tool in zHealthEHR that will allow you ...Insurance Claim Error Cheat Sheet
In chiropractic billing, claim errors result in either rejections or denials and overcoming these can be challenging. Even small errors like missing or incorrect patient demographic information can lead to claim denials and payment delays. As a ...How to Rebill or Resubmit Claims
In this help guide, we will show you how you can resubmit a claim both through the ERA as well as manually through Patient Billing. Once your claim has been submitted to the insurance, the claim comes back as an ERA or through email as an EOB. Once ...